Network Management
PreferredOne Expands Preferred Provider Organization (PPO) Network Access in Minnesota and North Dakota
PreferredOne is pleased to announce beginning January 1, 2017, Aetna will begin accessing the PreferredOne PPO network for its members in Minnesota and North Dakota. The PreferredOne PPO network includes 99 percent of Minnesota and North Dakota hospitals and clinics.
This change will not affect the way in which providers submit claims, verify member eligibility, access claim information, etc. Those services & functions will all continue to be handled directly through Aetna. Please continue to access information online from Aetna and submit your claims to Aetna as you have been with the current network. Watch this newsletter and the Aetna newsletter for any product, policy, and process updates on the Aetna business. If you have any questions or concerns, please contact your Provider Rep at PreferredOne.
One difference you will see from the other PreferredOne PPO business is that in January if your contract is not loaded into Aetna’s system, PreferredOne will not be able to hold claims for you (you will be submitting claims directly to Aetna). Providers will be responsible for holding Aetna claims temporarily (for contracts with a 1/1/2017 effective dates) until Aetna completes their process of loading the new rates. If claims are submitted to Aetna prior to your 1/1/2017 contract being loaded into their system, claims will be paid at the previous year’s rates. There will be no reprocessing of claims. So please be sure to check with Aetna that your new rates are loaded for 1/1/2017 before you release claims for those dates of service on or after 1/1/2017.
For questions or clarification please contact your Contract Manager or Provider Rep directly.
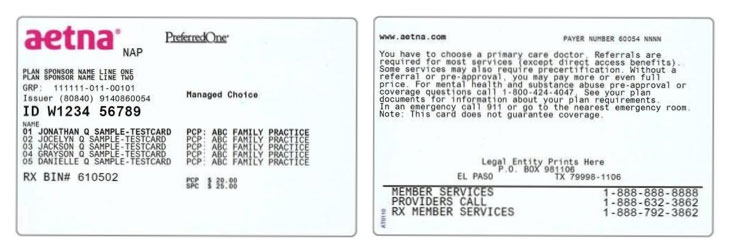
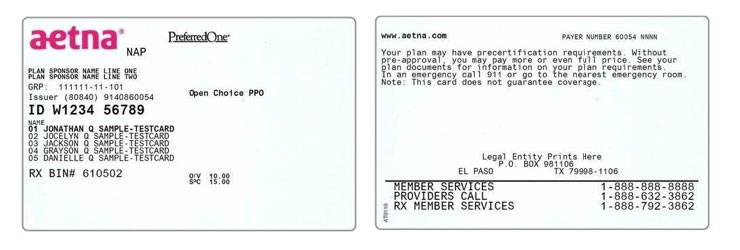
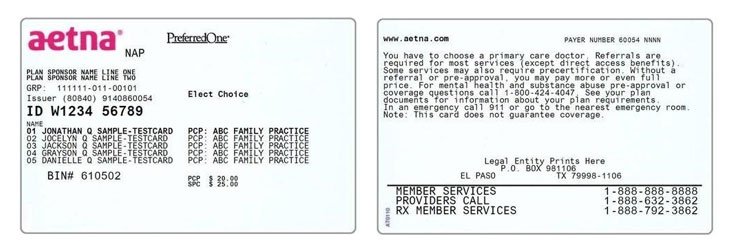
PreferredOne/Aetna Sample Member ID Cards
2017 Fee Schedule Update
Professional Services
PreferredOne’s Physician, Mental Health and Allied Health Fee Schedules are complete and will become effective for dates of service beginning January 1, 2017. These changes are expected to be an increase in overall reimbursement. As with prior updates, the effect on physician reimbursement will vary by specialty and the mix of services provided.
Physician fee schedules will be based on the 2016 CMS Medicare physician RVU file without geographic practice index (GPCI) applied and without the work adjuster applied, as published in the Federal Register May 2016. New codes for 2017 will be based on the 2017 CMS Medicare physician RVU file without geographic practice index applied and without the work adjuster applied as published in the Federal Register November 2016. Other new non-RVU based codes will be added according to PreferredOne methodology. The fee schedules for other provider types (such as allied, PhD, Masters and BA) will also be updated.
Various fees for services without an assigned CMS RVU have been updated accordingly. New codes that are not RVU-based will also be added. Examples of these services include labs, supplies/durable medical equipment, injectable drugs, immunizations and oral surgery services. The lab methodology as a % of CMS will remain the same for all products. PreferredOne will maintain the current default values for codes that do not have an established rate.
The 2017 Physician fee schedules will continue to apply site of service differential for RVU –based services performed in a facility setting (Place of Service 10, 21-25 are considered facility).
The Convenience Care Fee and Dental schedules will also be updated January 1, 2017. New codes were added to this fee schedule and reminder that any code not on the fee schedule will not be reimbursed.
New ASA codes for Anesthesia services will be updated with the 2017 release of Relative Value Guide by the American Society of Anesthesiologists. This update will take place by January 1, 2017.
Requests for a market basket fee schedule may be made in writing to PreferredOne Provider Relations. Reminder that new codes for 2017 will be added to all fee schedules using the above listed methodology. PreferredOne reserves the right to analyze and adjust individual rates throughout the year to reflect current market conditions. Any changes will be communicated via the “PreferredOne Provider Bulletin”.
Hospital Services/UB07/Outpatient Fee Schedules
The 2017 Calendar year DRG schedule will be based on the CMS MS-DRG Grouper Version 34 as published in the final rule Federal Register to be effective October 2016.
For those on Ambulatory Payment Classifications (APC), we are using Optum hospital-based grouper that will be one year lag. For example, for 2017 rates, PreferredOne may use the 2016 APC grouper and edits and weights as of October 2016.
The Facility (UB04) CPT fee schedule will consist of all physician CPT/HCPC code ranges and will be based on the 2016 CMS Medicare physician RVU file, without the geographic practice index applied and without the work adjust applied. The global rules for the facility CPT fee schedule are as follows:
- The surgical codes (10000 – 69999 and selected HCPCS codes including, but not limited to G codes and Category III codes) are set to reimburse at the practice and malpractice RVU’s
- Office visit codes (i.e. 908xx, 99xxx code range) are set to reimburse at the practice expense RVU’s
- Therapy codes are set at the Allied Health Practitioner rates
- For those codes that the Federal Register has published a technical component (TC) rate. This rate will be set as the base rate.
- All other remaining codes are set to reimburse at the professional services established methodology.
Reminder that new codes for 2017 will be added to all fee schedules using the above listed methodology. PreferredOne reserves the right to analyze and adjust individual rates throughout the year to reflect current market conditions. Any changes will be communicated via the “PreferredOne Provider Bulletin”.
Off-Cycle Fee Schedule Updates
Other provider types such as DME, Home Health, Skilled Nursing Facility updates will take place April 1, 2017.
Pricing and Payment Policies
New:
#18 Modifer Payment Reductions
#21 Reimbursement for Add on Codes without Primary Code
#22 Brain CT billed same date of service as Sinus CT
#25 Incremental Nursing Services
#26 Robotic Assisted Surgery S2900
Revised Coding Reimbursement Policy:
#18 Reimbursement for Surgical Trays
MEDICAL MANAGEMENT
Affirmative Statement about Incentives
PreferredOne does not specifically reward practitioners or other individuals for issuing denials of coverage or service care. Financial incentives for utilization management decision-makers do not encourage decisions that result in under-utilization. Utilization management decision making is based only on appropriateness of care and service and existence of coverage.
Medical Policy Updates
The Integrated Health and Pharmacy and Therapeutics Quality Management Subcommittees approve new criteria sets for use in their respective areas of Integrated Healthcare Services. Quality Management Subcommittee approval is not required when there has been a decision to retire a PreferredOne criteria document or when medical polices are created or revised; approval by the Chief Medical Officer is required. The Quality Management Subcommittees are informed of these decisions.
For the most current versions of the Medical Policy documents, please access the Medical Policy section on the PreferredOne website. (Click on Benefits and Tools then choose Medical Policy, Precertification, Prior Authorization.) Medical Policy documents are available on the PreferredOne website to members and to providers without prior registration.
Since the last newsletter, the following are the new, revised, or retired Medical Policy documents. Some of the more extensive Medical Policy updates are detailed for a few of the items below. If you wish to have paper copies of these documents, or you have questions, please contact the Medical Policy Department telephonically at (763) 847-3386 or online at Heather.Hartwig-Caulley@PreferredOne.com.
Durable Medical Equipment, Prosthetics, Orthotics, and Supplies List
- Breast pumps (manual and electric) – The following statement was added: “Purchase of a manual or standard electric breast pump medically necessary during pregnancy or at any time following delivery for breastfeeding.”
- Diabetic equipment/monitors – Removed “initial placement” verbiage related to Continuous Glucose Monitors. Prior authorization is required for replacement also. Prior authorization is not required for the provision of supplies.
- Repair, replacement, revision of eligible DMEPOS item – The following statement was added: “If the DMEPOS item requires prior authorization, the replacement also requires prior authorization.”
Integrated Health
- Revised Criteria
- MC/A006 Ventricular Assist Devices – Revisions were made to capture the FDA approved indication for the use of these devices in children.
- MC/B003 Orthodontic Services – Revisions were made to reflect that the malocclusion has to be related to a medical condition for coverage of orthodontic treatment under the medical benefit; to require medical necessity in addition to dental necessity, and to raise the Salzmann scoring requirements from 25 to 42.
- MC/F021 Bone Growth Stimulators (Osteogenic): Electrical and Ultrasonic – Revisions were made to now include coverage for the use of bone growth stimulators in the cervical spine.
- MC/G011 Hyperbaric Oxygen Therapy – Revisions were made to capture coverage and medical necessity guidelines for the use of Hyperbaric Oxygen Therapy for Idiopathic Sudden Sensorineural Hearing Loss.
- MC/T001 Bone Marrow/Stem Cell Transplantation – Revisions were made to clarify when more information regarding disease severity is required (ie, in absence of protocol or off protocol
- MC/T003 Heart Transplantation – Added specific indications for heart transplantation in conjunction with the requirement of meeting protocol. Also revised to clarify when more information regarding disease severity is required (ie, in absence of protocol or off protocol).
- MC/T004 Liver Transplantation - Added specific indications for liver transplantation in conjunction with the requirement of meeting protocol. Also revised to clarify when more information regarding disease severity is required (ie, in absence of protocol or off protocol).
- Revised Policies
- MMP/D009 Dental Services, Hospitalization, and Anesthesia for Dental Services Covered Under the Medical Benefit – Revisions were made to ensure that any treatment associated with a dental service due to an accidental injury must be started and completed within the timeframes outlined in the applicable SPD/COC.
Investigative List
- Additions
- Gene Expression Profiling and/or molecular testing for cancers of unknown primaries/occult primary tumors.
- Gene Expression Profiling and/or molecular testing for colorectal cancer.
- Gene Expression Profiling and/or molecular testing for predicting malignancy in women with adnexal mass, includes, but not limited to, OVA1 and Risk of Ovarian Malignancy Algorithm (ROMA).
- Revisions
- To Hyperthermia Treatment – This entry was revised to allow cytoreductive/debulking surgery combined with hyperthermic intraperitoneal chemotherapy (HIPEC) for isolated peritoneal metastases from colon cancer when R0 resection can be achieved and when performed at experienced centers by high volume providers with demonstrated expertise.
- Tumor Necrosis Factor (TNF) antagonists serum drug concentration and antibody testing – This entry was revised to widen the investigative position to also include serum drug concentration and antibody testing for all TNF antagonists
Pharmacy and Therapeutics
- New Criteria
- PC/S005 Synagis Prior Authorization
- Revised Criteria
- PC/A003 Combination β2-Agonist/Corticosteroid Inhalers Step Therapy – Since branded and generic metaproterenol are no longer available, they were deleted from Table 1.
- PC/A005 Antidepressant Medications Step Therapy – Tables 1 and 2 were revised to reflect that Pristiq will now be first line.
- PC/B009 Bisphosphonates and Osteoporosis Prevention and Treatment Medications – The Purpose statement was revised to require trial of medications with different mechanisms of action prior to approval of higher line medications.
- PC/N002 Nasal Corticosteroids Step Therapy – The Purpose statement was revised to change the requirement of number of first-line medications that must be trialed. Tables 1 and 2 were revised to reflect changes in generic availability and change in FDA-approved age for Qnasl. Deletions were made to the Exception statements due to the change in generic availability in the class.
- PC/R004 Rituxan Prior Authorization (Non-Oncology) – Treatment for Hemophilia factor inhibitors was deleted due to the lack of evidence regarding the off-label use of Rituxan for this indication. Future requests will be considered on a case-by-case basis, following the Pharmacy Off-label process.
- Retired Policies
- PP/P001 Bypass of Prior Authorization of Medications Ordered by a Contracted Specialist
New Authorization Forms
A Synagis (palivizumab) Authorization Form and an Infusion Authorization Form have been recently developed and are now available on the PreferredOne website (under Provider/Provider Forms). It is important that the forms are completed as clearly and specifically as possible. Incomplete or illegible forms may result in the return of the form for further completion or clarification and a delay in processing the request. Both forms and other relevant documents must be faxed to (763) 847-4014.
Also, a reminder, PreferredOne will require prior authorization for the use of Synagis (palivizumab) beginning with the 2016 respiratory syncytial virus (RSV) season. The newly developed Synagis Prior Authorization criteria document (PC/S005) is available on the PreferredOne website.
Remember to check the Prior Authorization List posted on the PreferredOne website. The list is located with the other Medical Policy documents on the PreferredOne internet home page. The list will be fluid, as we see opportunities for impact driven by, but not limited to, new FDA-approved devices, medications, technologies, or changes in standard of care. Please check the list regularly for revisions.
Flu Mist
Due to the recent CDC’s Advisory Committee on Immunization Practices (ACIP) position that the live attenuated influenza vaccine (LAIV), also known as the “nasal spray” flu vaccine, should not be used during the 2016-2017 flu season, PreferredOne will not be covering this vaccine until such time as ACIP changes their recommendation.
ACIP continues to recommend annual flu vaccination, with either the inactivated influenza vaccine (IIV) or recombinant influenza vaccine (RIV), for everyone 6 months and older.
Low-dose Computed Tomography
Effective 9/15/2016, PreferredOne will only allow low-dose computed tomography, HCPCS G0297 or S8032, at the preventive benefit level for lung cancer screening.
Quality Management
Clinical Practice Guidelines
PreferredOne supports the Institute for Clinical Systems Improvement’s (ICSI) mission and promotes clinical practice guidelines to increase the knowledge of both our members and contracted providers about best practices for safe, effective and appropriate care. Although PreferredOne endorses all of ICSI’s guidelines, it has chosen to adopt several of them and monitor their performance within our network (Clinical Practical Guidelines). The guidelines that PreferredOne’s Quality Management Committee has adopted include ICSI’s clinical guidelines for Coronary Artery Disease, Asthma, Depression, ADHD/ADD, Prenatal - Routine Care, Preventive Services for Children and Adolescents, and Preventive Services for Adults. The performance of these guidelines by our network practitioner's is monitored utilizing HEDIS and Minnesota Community Measurement data. The most recent version of the ICSI guidelines that we have adopted can be found on ICSI's website at www.icsi.org.
Preventive Health Services for Children and Adolescents
The ICSI Preventive Health Services for Children and Adolescents guideline provides the basis for measurement and monitoring of several relevant clinical indicators. The measures that are assessed for adherence to the clinical guideline include the spectrum of childhood immunizations (using HEDIS technical specifications) and Chlamydia screening for adolescents (using HEDIS technical specifications). Utilizing 2015 claims data PreferredOne evaluated adherence to this set of guidelines through our HEDIS data collection process. The results for the entire PreferredOne network were as follows:
Preventive Health Measures for Children & Adolescents 2015 |
|
Four DTaP/DT |
87.08% |
Three IPV |
90.17% |
One MMR |
92.42% |
Three Hib |
91.57% |
Three Hepatitis B |
90.45% |
One VAR, or documented chicken pox disease |
89.61% |
Four pneumococcal |
86.52% |
Two Hepatitis A |
88.48% |
Rotavirus |
81.74% |
Two influenza |
67.42% |
Chlamydia screening |
43.96% |
PreferredOne strongly encourages our provider network clinic systems to send their immunization information to the Minnesota Immunization Information Connection (MIIC). MICC data is utilized to support our HEDIS data collection process and may reduce the burden of chart review at your clinic. To learn more about MICC and how you can participate please visit: http://www.health.state.mn.us/miic.
Continuity & Coordination of Care
Continuity and coordination of care is important to PreferredOne. If your clinic is terminating your contract with PreferredOne please notify your PreferredOne provider representative immediately. According to the Minnesota Department of Health statute 62Q.56 subdivision 1: the health plan must inform the affected enrollees about termination at least 30 days before the termination is effective, if the health plan company has received at least 120 days’ prior notice. If you need further information please contact your network representative at PreferredOne regarding this statute.
Case Management Referral
What is Case Management?
Case management is a collaborative process among the Case Manager (an RN or Social Worker), the plan member, and the member’s family and health care providers. The goal of case management is to help members in navigating through the complex medical system. The Case Manager will assist in preventing gaps in care with the goal of achieving optimum health care outcomes in an efficient and cost-effective manner. This service is not intended to take the place of the attending providers or to interfere with care.
Core Services
- Serve as a resource to members
- Provide both verbal and written education regarding a disease condition
- Coordinate care to promote compliance with provider treatment plan
- Serve as a liaison between the health plan, member and providers
Eligibility and Access
All members of the health plan experiencing complex health needs are eligible for case management. A Case Manager may call out to a member based on information that has been received at PreferredOne or members may call and request a Case Manager. There is no cost for this service and it is strictly optional.
Health care provider referrals and member self referrals are accepted by contacting PreferredOne and requesting to speak with a Case Manager. The telephone number for the case management department is 763-847-4477, option 4.
Programs from PreferredOne at No Cost to Your Patients
PreferredOne has implemented Chronic Illness Management and Treatment Decision Support programs available to your patients who live with chronic conditions. Your patients will still have the same level of benefits, access to any ancillary services and access to your referral network. They will also continue to see their practitioner(s) and receive the same services that they currently provide them.
The Chronic Illness Management (CIM) and Treatment Decision Support (TDS) Programs focus on the following conditions;
CIM:
- Diabetes
- Coronary Heart Disease
- Congestive Heart Failure
- Chronic Obstructive Pulmonary Disease
- Asthma (adult and juvenile)
- Multiple Sclerosis
- Rheumatoid Arthritis
- Ulcerative Colitis
- Crohn’s Disease
- Rare conditions (Sickle Cell, Cystic Fibrosis, Lupus, Parkinsons, Myasthenia Gravis, Hemophilia, Scleroderma, Dermatomyositis, Myositis, Polymyositis, CIDP, ALS, and Gaucher Disease)
TDS:
- Low Back Pain
- Health Mom and Baby
The goals of these programs are to:
- Promote self-management of chronic conditions.
- Improve adherence to treatment plans.
- Improve adherence to medication regimes.
- Reduce or delay disease progression and complications.
- Reduce hospitalizations and emergency room visits.
- Improve quality of life.
Benefits to You and Your Practice
These PreferredOne programs are designed to collaborate with a practitioner’s recommended treatment plans. With the help of a nurse health coach, patients are educated telephonically about their chronic conditions and taught how to track important signs and symptoms specific to their condition. There are several benefits when your patients participate in these PreferredOne programs:
- Program participants learn how to better follow and adhere to treatment plan
- Program participants learn how to maximize their office visits
- If clinically concerning warning signs are discovered through the program, practitioners are notified, if clinically appropriate, via a faxed Health Alert
- Program participants receive ongoing support and motivation to make the necessary lifestyle changes practitioners have recommended to them
Benefits to Patients
- Access to a PreferredOne Registered Nurse or Social Worker
- Information about managing their health condition
- Education and tools to track their health condition
- Equipment, as needed, for participation in the program
- Access to Healthwise®, an online health library at www.preferredone.com
Program Participants learn to:
- Track important signs and symptoms to detect changes in their health status early enough to avoid complications and possible hospitalizations
- Make better food choices
- Start an exercise program
- Regularly take their medications
- Avoid situations that might make their condition worse
To make a Referral to the PreferredOne CIM or TDS programs:
Contact PreferredOne toll free at 1-800-940-5049 Ext. 3456. Monday-Friday 7:00am to 7:00pm CST.
Do you have a doctor who is not accepting new patients?
PreferredOne is requesting all physicians to submit information regarding acceptance of new patients. If you are a clinic site who has a physician that is not accepting new patients you can go to www.PreferredOne.com, select For Providers, login, select Your Clinic Providers and edit the Accepting New Patients information for your provider. Our provider directories will be updated with this information.
If you are unable to access the provider secured website please send an alert to PreferredOne by electronic mail to quality@preferredone.com. We would ask that you please include your clinic(s) site name and address, the practitioner(s) name and NPI number who are no longer accepting new patients and the contact information for the individual sending us the notification in case we have questions.
Quality Complaint Reporting for Primary Care Clinics
MN Rules 4685.1110 and 4685.1900 require health plans to collect and analyze quality of care (QOC) complaints, including those that originate at the clinic level.
A QOC complaint is any matter relating to the care rendered to the member by the physician or physician’s staff in a clinic setting. Examples of QOC include, but are not limited, to the following:
- Clinical practitioner/provider – knowledge or skill, behavior, attitude, diagnosis and treatment, violation of member’s rights, etc.
- Non-clinical staff/facility – competence, communication, behavior, environment (cleanliness, lacking areas for confidential communications, unsafe), violation of member’s rights, etc.
QOC complaints directed to the clinic are to be investigated and resolved by the clinic, whenever possible. PreferredOne's requires clinics to submit quarterly reports to our Quality Management Department as specified in the provider administrative manual. We have attached the form for your reference. If you'd like to have the file electronically please e-mail quality@preferredone.com. If you have any questions or concerns please contact Arpita Dumra at 800-940-5049, ext. 3564 or e-mail arpita.dumra@preferredone.com. (Quality Complaint Form)
